Article added / Artikel hinzugefügt 01.10.2021
Generally Articles and Discussions about Osteosarcoma in Dogs
→ Evaluations of phylogenetic proximity in a group of 67 dogs with
osteosarcoma: a pilot study
Article added / Artikel hinzugefügt 01.10.2021
Generally Articles and Discussions about Osteosarcoma in Dogs
→ Canine Periosteal Osteosarcoma
Images added / Abbildungen hinzugefügt 02.05.2019
Generally Sonography Atlas of Dogs →
Cardiovascular system → Pulmonary vessels
New subcategory added / Neue Unterkategorie hinzugefügt 02.05.2019
Generally Sonography Atlas of Dogs →
Cardiovascular system → Pulmonary vessels
Images added / Abbildungen hinzugefügt 01.05.2019
Generally Sonography Atlas of Dogs →
Cardiovascular system → Heart valvular diseases



Contrast-enhanced ultrasonography (CEUS) in canine liver examination

M. Wdowiak, A. Rychlik, R. Nieradka, M. Nowicki
Department of Clinical Diagnostics,
University of Warmia and Mazury M. Oczapowskiego 14, 10-719 Olsztyn, Poland
DOI 10.2478/v10181-010-0007-2
Abstract
Ultrasonography is a noninvasive diagnostic tool used to image size, shape, parenchyma and
vascularization of various body organs. Unfortunately, the ultrasonographic image is characterized by
a low contrast due to similar acoustic properties of the soft tissue. The Doppler mode provides
information about blood flow, but is incapable of imaging small vessels and capillaries because of
their low blood flow velocity (1 mm/s). However, a possibility to increase the effectiveness of ultrasonographic diagnostics exists, thanks to intravenous ultrasound contrast agents (UCAs)
consisted of
gas microbubbles.
The purpose of this review paper is to characterize specific imaging techniques necessary to
conduct a contrast-enhanced liver examination and indications for CEUS as an alternative diagnostic
method.
Specific contrast-enhanced imaging techniques
The basic B-mode (Haers and Saunders 2009) is not effective enough for ultrasound contrast agent detection in tissue, so it can not be used in contrast-enhanced ultrasonography (CEUS). All
Doppler modalities are too sensitive to the microbubbles and this hypersensitivity causes artifacts such as “color blooming” (color Doppler) and “flash” (power Doppler), which decreases the
usefulness of these modes. “Color blooming” artifact (Nilsson 2001) presents
itself as extravascular color induced by reverberation and/or a high gain setting. The “flash” artifact appears
when tissue or transducer movement disturbs the desired flow signal. Specific contrast-enhanced imaging techniques (Haers and Saunders 2009) are deprived of these defects and bring satisfying
clinical results and artifact
reduction. Many techniques have been created e.g. second harmonic imaging, pulse/phase inversion harmonic imaging, cadence-contrast pulse sequencing and power (amplitude)
modulation.
These specific imaging techniques take advantage of the nonlinear properties of UCAs which manifests in asymmetrical oscillation of the gas microbubbles under ultrasonic wave influence. The
nonlinear properties of UCAs (Quaia 2007) increase contrast detection in tissues, thus increasing the contrast to tissue ratio and decreasing artifacts and noise.
The principles of the second harmonic imaging are to create an image based on a frequency twice the value of the wave emitted by the transducer. The fundamental wave is filtered. If the
fundamental wave is 2 MHz, then the second harmonic is 4 MHz, third harmonic 6 MHz and so on. Conventional USG systems emit and receive sound waves with identical frequencies. On the contrary to
conventional methods (Szatma´ri et al. 2003), second harmonic imaging receives echoes of twice the frequency than the fundamental pulse. The limitations of this technique are low
spatial axial resolution and a possibility of contrast resolution reduction if the transmit pulse bandwidth
and the receive bandwidth overlap (harmonic signal contamination). Harmonic imaging (O’Brien and Holmes 2007, Quaia 2007) improves the “good artifacts” (shadow and through transmission –
diagnosis of mineralization and fluid) and reduces the “bad” artifacts (ring-down).
Pulse (phase) inversion (Szatma´ri et al. 2003) imaging also is based on harmonic frequencies, but every other emitted pulse is inverted. The two subsequent echoes are added and each scanning
line consists of two pulses. The added tissue echoes are nulled, but the echoes from the “nonlinear” microbubbles’ are not. This results in a strong harmonic signal. The advantages of this
technique (Stewart and Sidhu 2006, Quaia 2007), are good spatial resolution
and no transmission spectrum restrictions. The disadvantage is a reduction in frame rate due to the need to interrogate each scan line twice.
Cadence-contrast pulse sequencing (CPS) is a technique developed by Siemens, which principles are to emit a sequence of sound waves effects in microbubble oscillation, and the echoes originating
from the microbubbles are filtered from tissue echoes by computer software. This technique (Quaia 2007) uses amplitude and phase modulation, and enables the visualization of all nonlinear
contrast response, even the strong, nonlinear fundamental frequency. This technique (O’Brien and Holmes 2007) allows imaging with higher frequencies resulting in increased
spatial resolution with the disadvantage of decreased temporal resolution. CPS, pairing the linear fundamental signal beside the nonlinear fundamental image, also allows anatomical
orientation.
Power (amplitude) modulation (Quaia 2007) – in every scanning line two pulses are emitted, one with half and the other with a full frequency. Then, the received echoes are subtracted in the
scanner to separate microbubble and tissue signals.
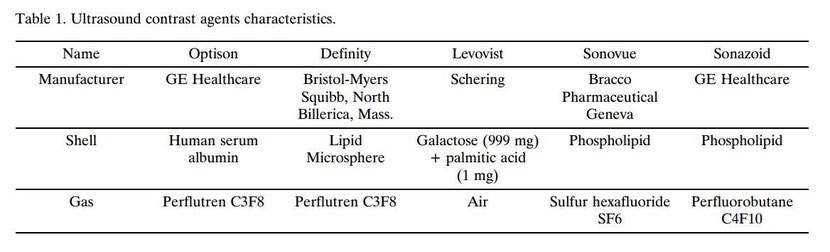
Ultrasound contrast agents (UCAs)
The first efforts (Calliada 1998) to enhance ultrasonic signals were based on i.v. admission of agitated 0.9% NaCl and receive sound wave reflections from the air microbubbles diluted in the
patients blood. Feinstein continued research in this field and discovered that blood albumins improve microbubble stability. His investigations resulted in the development of the first
pharmaceutical contrast agent, AlbunexTM. The first echo-enhancing substances were
applied in cardiology and were incapable of penetrating the pulmonary bed. Ultrasound contrast media (Nyman et al. 2005) are classified into two generations according to the gas present inside
the microbubbles: I gen agents (Albumex, Levovist) contain air, while II gen agents contain perfluorocarbon or sulfur hexafluoride (SonoVue, Optison, Definity).
New generation UCAs consist of small, gas-filled, mainly by prefluorane derivatives of saturated hydrocarbons (e.g. perfluoropropane, perfluorohexane, octafluoropropane) microbubbles stabilized
by an external shell (denaturated human albumin, surfactant or phospholipids). The gas enhances the sound wave reflection and the gas type determines the quality of enhancement and microbubble
durability. Gases with high molecular mass are poorly dissolved in serum thus are more durable and extend the enhancement effect. The shell determines elasticity which allows the ability of
oscillation in a ultrasonic field and a more effective and longer enhancement effect.
The diameter (Szatma´ri et al. 2003) of the microbubbles (1-7 μm) is smaller than the red blood cells diameter; this excludes the possibility of capillary embolization. In comparison to contrast
agents used in computer tomography or magnetic resonance imaging, UCAs remain in the intravascular space and do not diffuse outside blood vessels. Not all UCAs (Nyman et al. 2005) allow the
imaging of the third, delayed phase (parenchymal, Kuppfer). This probably
depends (Stewart and Sidhu 2006, Kanemoto et al. 2008) on UCAs elimination by phagocytes, e.g. Sonazoid (99% is phagocytosed) and Levovist (47% is phagocytosed) image the parenchymal phase, but
Sonovue does not.
CEUS clinical applications
Contrast-enhanced ultrasonography (Haers and Saunders 2009) is mainly used to evaluate the liver and spleen. Other organs in case of which CEUS is useful are the kidneys, pancreas, lymph nodes
and portal systemic shunts (PSS) diagnostics. CEUS liver evaluation consists of lesion detection (mainly focal, but also diffuse), lesion characteristics and monitoring after tumor
resection.
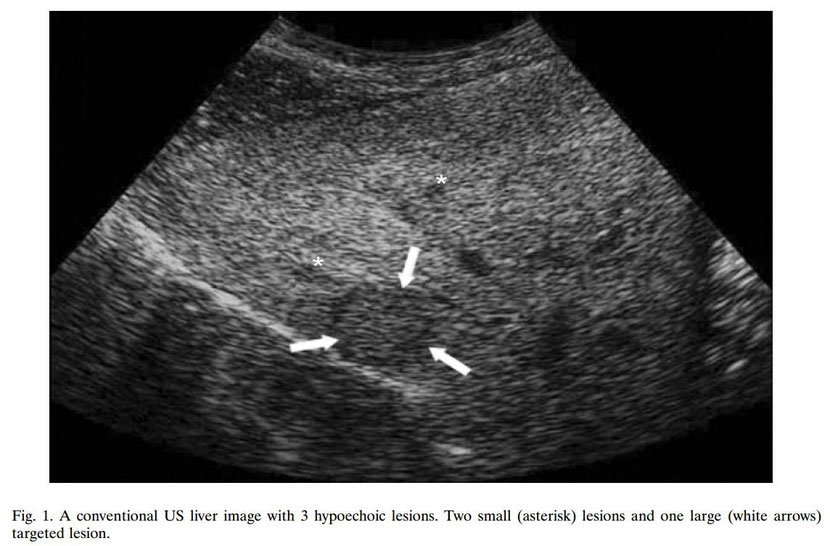
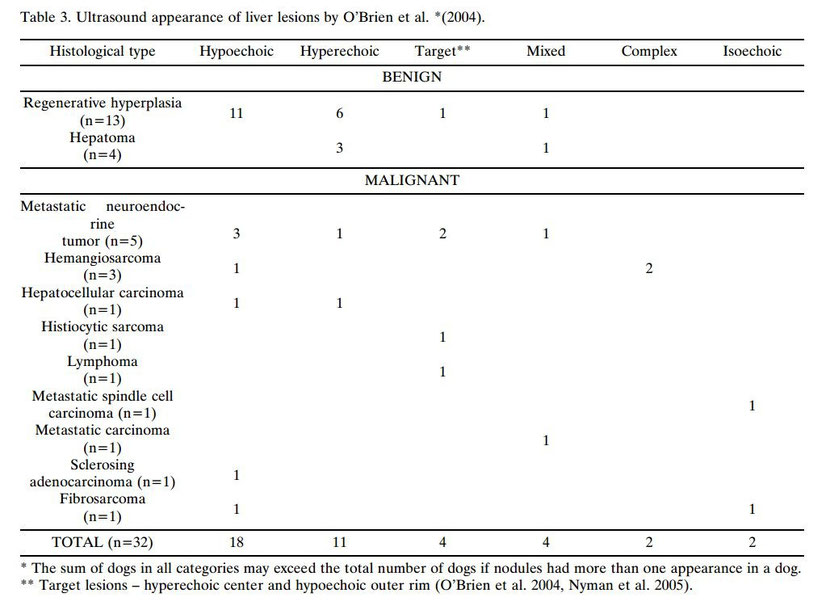
Liver examination – the examination of focal lesions is the main CEUS indication in the canine and feline patient. The evaluation of focal lesions (Haers and Saunders 2009) by conventional
ultrasonography is based on lesion morphology (echogenicity) and blood flow parameters (Doppler mode – hyper/hypovascularization). This enables the diagnose of liver cysts (anechogenic) or
calcifications (acoustic shadow), but not always liver soft tissue lesions.
Hepatic nodules are common in dogs, focal nodular hyperplasia (FNH) occurs in 70% of the canine population over the age of six, and in all dogs over 14 years of age. Other causes of hepatic
nodules (O’Brien et al. 2007, Haers and Saunders 2009) are haematomas, abscesses, focal hepatic necrosis, primary neoplasm (hepatocellular carcinoma, cholangiocellular carcinoma, sarcoma,
carcinoid) and metastases (hemangiosarcoma, pancreatic cancer, neuroendo- crine tumors). The assessment of liver lesions in CEUS is based on two necessary elements: lesion detection and lesion
characteristics. After a lesion is detected (O’Brien et al. 2007, Haers and Saunders 2009) a description (lesion characteristics) is useful in differentiating between neoplasm/non neoplasm
lesions, benign/malignant neoplasm, and even between certain types of malignant tumors.
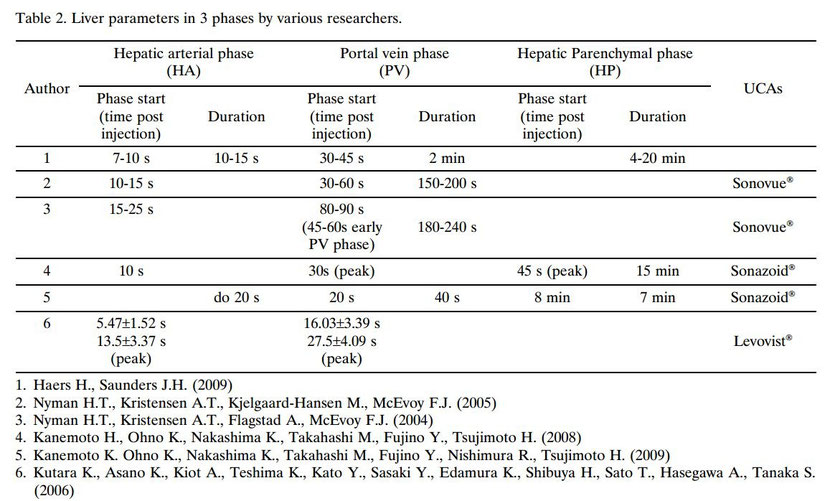
The CEUS pattern of healthy dogs has been described. As a result of the double vascularization of the hepatic tissue by the hepatic artery (20% to 30% of blood) and the portal vein (70% to 80% of
blood), the following phases have been described (Nyman et al. 2004, Kutara et al. 2006, Kanemoto et al. 2008, Kanemoto et al. 2009, Haers and Saunders 2009):
1. Hepatic arterial phase (HA) – enhancement of the hepatic artery and its tributaries – begins at 7 to 10 seconds post UCAs injection and has a duration time of 10 to 15
seconds.
2. Portal vein phase (PV) – begins at 30 to 45 seconds post UCAs injection, duration time up to 2 minutes post injection. In cirrhotic patients (Szatma´ri et al. 2003) a delay is
possible.
3. Hepatic parenchymal phase (HP) – also known as the Kuppfer or delayed phase – enhancement of the hepatic parenchymal sinusoids – lasts until the UCAs are eliminated from the parenchyma, about
4 to 20 minutes, depending on contrast agent type.
Lesion detection – CEUS (Haers and Saunders 2009) is useful in detecting small and unclear malignant or isoechoegenic lesions, which are often invisible on a conventional USG
image.
The liver is frequently the first organ in which neoplasm’s metastasize from primary tumors in the abdominal cavity by blood vessels (Nyman et al. 2005). The presence of a metastatic tumor with a
diameter of 1.5 cm results in portal hypertension (blood vessel compression theory). To maintain a constant blood flow (Nyman et al. 2005) (energy)
the metastasis supplements its shortage from the hepatic artery or by arteiovenous shunts. The CEUS image (Nyman et al. 2005) of metastatic tumors is various and is characterized by: a vascular
ring, growing peripheral, necrotic center and various degree of calcification and density.
The effectiveness of ultrasonic imaging of hepatic lesions (Nyman et al. 2005) with a diameter smaller than 2 cm (depending on the information source) is 53% to 84%. The sensitivity for nodular
lesions below 1 cm in diameter is 20%. The presumed threshold for detection is 0.5 cm.
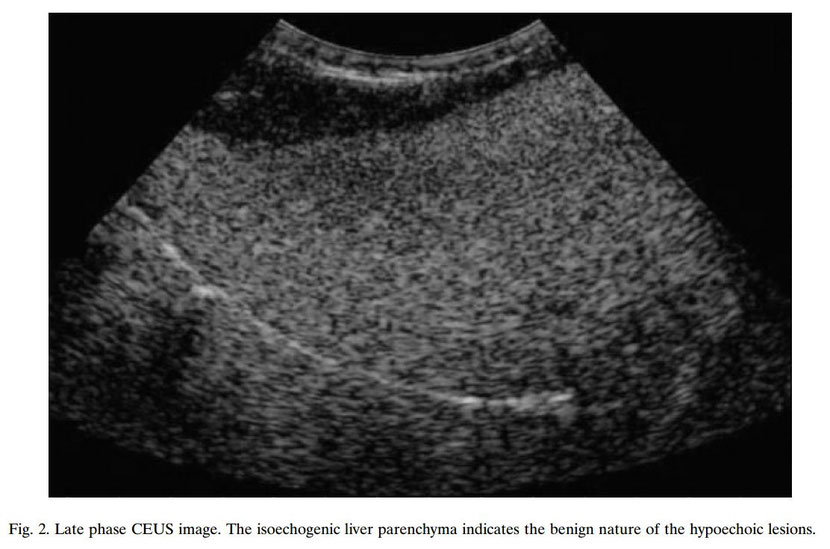
Lesion characteristics – the change in enhancement throughout the phases gives a basis to focal hepatic lesion diagnosis. The arterial phase (Haers and Saunders 2009) provides information about
the degree and pattern of vascularization, while the portal vein and parenchymal phases inform about UCAs elimination. Most benign lesions are characterized by a constant enhancement. This
determines that the focal lesion is enhanced in a degree equal or higher than the hepatic parenchyma during the portal vein phase. Thus, benign lesions can be differentiated
from most malignant lesions which are strongly enhanced in the early, hepatic artery phase, and poorly enhanced and hypoechogenic to the hepatic parenchyma in the portal vein and parenchymal
phase (early washout phenomenon). This is due to the malignant tumors blood supply, the hepatic artery.
Focal hepatic lesion characteristics in dogs have been described in three phases (Kanemoto et al. 2009):
1. Hepatic arterial phase – degree of vascularization in comparison to the hepatic parenchyma (hyper-/iso-/ hypovascular).
2. Portal vein phase – lesion perfusion (hyper-/iso-/hypoperfusion).
3. Hepatic parenchymal phase – echogenicity enhancement was classified as no lesion presence, unclear lesion or clear lesion visualization in the hepatic parenchyma.
The study was conducted on 25 dogs, 16 had malignant lesions and 9 benign lesions; 6 dogs with hepatocellular carcinoma (HCC), 3 with cholangiocellular carcinoma (CCC), 1 with leiomyosarcoma, 1
with liposarcoma, 1 with sarcoma of unknown origin, 1 with lymphoma, 1 with histiocytosis, 1 with mast cell tumor, 6 with nodular hyperplasia
HN and 3 with cirrhotic nodules.
The lesion characteristics in each phase are: 5/6 dogs with HCC were hypervascular in the arterial phase, 4/6 hyperperfusion was observered in the portal vein phase and 4/6 had a dysmorphic image in the parenchymal phase. In the parenchymal phase, an uncomplete, irregular or partially enhanced lesion was detected which is a HCC
mark.
Dogs with CCC: the lesion was hipoechogenic during the artery and portal vein phase in comparison to the hepatic parenchyma. The vascular pattern in the arterial phase was peripheral, rim-like. A
clear lesion was apparent in the parenchymal phase.
The hemopoietic tumors (lymphoma, malignant histiocytosis and mast cell tumor) were almost identical. Hypovascularity and early washout was observed in the arterial and venous phase. A stippled
vascular
pattern was observed in the dog with lymphoma, and a peripheral (rim pattern) vascular pattern characterized the malignant histiocytosis and the mast cell tumor. Clear parenchymal lesion was
observed.
Dogs with leiomyosarcoma and sarcoma of unknown origin: hypovascularity in the artery phase, early washout in the portal vein phase and a clear lesion in the parenchymal phase.
Liposarcoma is hypoechogenic to the hepatic parenchyma and has an unclear lesion image in the parenchymal phase.
Dogs with benign lesions (6 nodular hyperplasia HN and 3 cirrhotic nodules): 8/9 no lesions visible in the parenchymal phase. Five out of six dogs with HN had a diffused and homogenic pattern,
which was isoechogenic or hypoechogenic in the arterial phase. One dog had a decrease in vascularization and was aechogenic in the vessel phases and a clear lesion was imaged in the parenchymal
phase.
Three dogs with cirrhotic nodules had identical changes in all three enhancement phases with minimally hypoechogenic characteristics.
O’Brien (2007) on the basis of his studies stated that UCAs decrease the visibility of benign focal lesions, causing isoechogenicity in the ultrasonographic image during the enhancements peak.
Also the enhancement patterns of malignant lesions were totally different from benign lesions patterns. Namely, during the peak of parenchymal enhancement all malignant focal lesions were
hypoechogenic. This occurrence (O’Brien et al. 2004) correlates with the malignancy with a very high sensitivity, specificity, positive predictive value, negative predictive and accuracy (100%,
94.1%, 93.8%, 100% and 96.9%, respectively).
Quantitative CEUS examination via time-intensity curves
Quantification of UCAs (Nyman et al. 2005) is necessary for mathematical evaluation of the degree of tissue perfusion and the detection of diffused lesions in tissue. UCAs are used as markers for
the dynamic evaluation of organs such as the liver, brain and kidneys. The results presented as time-intensity curves for a ROI (region of interest) are calculated by built-in software installed
in ultrasound systems. The following parameters (Ziegler et al. 2003, Nyman et al. 2005) are computed: upslope, downslope, baseline, peak, change and time to peak and additionally: area under
curve (AUC), intensity peak (IP), and mean Transit Time (mTT). Arteriovenous UCAs transit times are digitally imaged as time-intensity curves which allow UCAs uptake and clearance measurement in
a ROI.
The shape of the time-intensity curve (Haers and Saunders 2009) is dependent upon the method of UCAs administration. A bolus injection causes a dual phase response, and a constant infusion is
characterized by a progressive enhancement with a subsequent plateau that persists until the end of the infusion.
Changes in vascuarization and blood flow secondary to pathological processes (Nyman et al. 2005, Haers and Saunders 2009) alternate the curves shape.
Comparison of CEUS with other Diagnostic Techniques CEUS, compared to contrast-enhanced CT or MRI (Stewart and Sidhu 2006, Haers and Saunders 2009), allows the analysis of tumor perfusion in
real-time without anesthesia. Additionally CEUS is more cost-effective, faster and does not involve ionizing radiation.
Compared with cytological examinations (Haers and Saunders 2009), CEUS is noninvasive and relatively easy to perform with the capability of differentiating benign and malignant
lesions.
In conclusion, contrast-enhanced ultrasonography is an alternative and competitive method to other imaging and cytological techniques.
Equipment
CEUS requires (Haers and Saunders 2009) a sophisticated ultrasound system, equipped with Doppler modalities, low frequency transducers of 1 to 3 MHz (such low frequencies are untypical for most
US systems used in veterinary medicine), software capable of specific contrast-enhanced imaging and eventually software for quantitative evaluation. Ultrasound contrast agents necessary for the
examination need to be reconstituted before usage. Route of administration is intravenous. The half-time of stability after reconstitution depends on the UCAs used (e.g. Definity 5 min, SonoVue
1h to 2 h, Sonazoid 2 h). To reduce costs, patients should be scheduled within the same period.
Conclusion
Contrast-enhanced ultrasonography increases the intensity of echo signals in the canine patient. The main indication for CEUS is focal liver lesion evaluation, especially differentiating between
benign and malignant lesions, and malignant lesion diagnosis.
Noninvasiveness, no anesthesia and the ability to evaluate in real-time are the main advantages of CEUS. The disadvantages are equipment requirements and cost of UCAs. Also the elimination of
contrast agents via lungs may limit the use of CEUS in patients with pulmonary diseases. Adverse effects were observed in human medicine after UCAs administration (headaches, diarrhea,
neutropenia, nausea, skin reactions, dyspnoe, rhinorrhagia). No adverse effects were observerd in animals.
References
Calliada F, Campani R, Bottinelli O, Bozzini A, Sommaruga MG (1998) Ultrasound contrast agents: basic
principles. Eur J Radiol 27: S157-S160.
Haers H, Saunders JH (2009) Review of clinical characteristics and applications of contrast-enhanced ultrasonography in dogs. J Am Vet Med Assoc 234: 460-470.
Kanemoto H, Ohno K, Nakashima K, Takahashi M, Fujino
Y, Nishimura R, Tsujimoto H (2009) Characterization
of canine focal liver lesions with contrast-enhanced
ultrasound using a novel contrast agent – sonazoid. Vet
Radiol Ultrasound 50: 188-194.
Kanemoto K, Ohno K, Nakashima K, Takahashi M, Fujino
Y, Tsujimoto H (2008) Vascular and Kupffer imaging of
canine liver and spleen using the new contrast agent
sonazoid. J Vet Med Sci 70: 1265-1268.
Kutara K, Asano K, Kiot A, Teshima K, Kato Y, Sasaki Y,
Edamura K, Shibuya H, Sato T, Hasegawa A, Tanaka
S (2006) Contrast harmonic imaging of canine hepatic
tumors. J Vet Med Sci 68: 433-438.
Nilsson A (2001) Artifacts in sonography and Doppler. Eur
Radiol 11: 1308-1315.
Nyman HT, Kristensen AT, Flagstad A, McEvoy FJ (2004)
A review of the sonographic assessment of tumor metastases in liver and superficial lymph nodes. Vet Radiol
Ultrasound 45: 438-448.
Nyman HT, Kristensen AT, Kjelgaard-Hansen M, McEvoy
FJ (2005) Contrast-enhanced ultrasonography in normal canine liver. Evaluation of imaging and safety parameters. Vet Radiol Ultrasound 46: 243-250.
O’Brien RT (2007) Improved detection of metastatic hepatic hemangiosarcoma nodules with contrast ultrasound
in three dogs. Vet Radiol Ultrasound 48: 146-148.
O’Brien RT, Holmes SP (2007) Recent advances in ultrasound technology. Clin Tech Small Anim Pract 22: 93-
-103.
O’Brien RT, Iani M, Matheson J, Delaney F, Young
K (2004) Contrast harmonic ultrasound of spontaneous
liver nodules in 32 dogs. Vet Radiol Ultrasound
45: 547-553.
Quaia E (2007) Contrast-specific ultrasound techniques.
Radiol Med 112: 473-490.
Stewart VR, Sidhu PS (2006) New directions in ultrasound:
microbubble contrast. Br J Radiol 79: 188-194.
Szatma´ri V, Harkhnyi Z, Vo¨ro¨ s K (2003) A review of nonconventional ultrasound techniques and contrast – enhanced ultrasonography of noncardiac canine disorders.
Vet Radiol Ultrasound 44: 380-391.
Ziegler LE, O’Brien RT, Waller KR, Zagrzebski JA (2003)
Quantitative contrast harmonic ultrasound imaging of
normal canine liver. Vet Radiol Ultrasound 44: 451-454.
Share this article / Teilen Sie diesen Artikel
Diese Webseite wurde mit Jimdo erstellt! Jetzt kostenlos registrieren auf https://de.jimdo.com